Tubal Ectopic Pregnancy: Laparoscopy vs. Laparotomy
Objectives: To compare the efficiency of laparoscopic treatment versus conventional abdominal surgery in the treatment of ectopic pregnancy (EP) and to review the clinical presentation, evaluate methods of diagnosis, and identifying the risk factors.
Abstract
Objectives: To compare the efficiency of laparoscopic treatment versus conventional abdominal surgery in the treatment of ectopic pregnancy (EP) and to review the clinical presentation, evaluate methods of diagnosis, and identifying the risk factors.
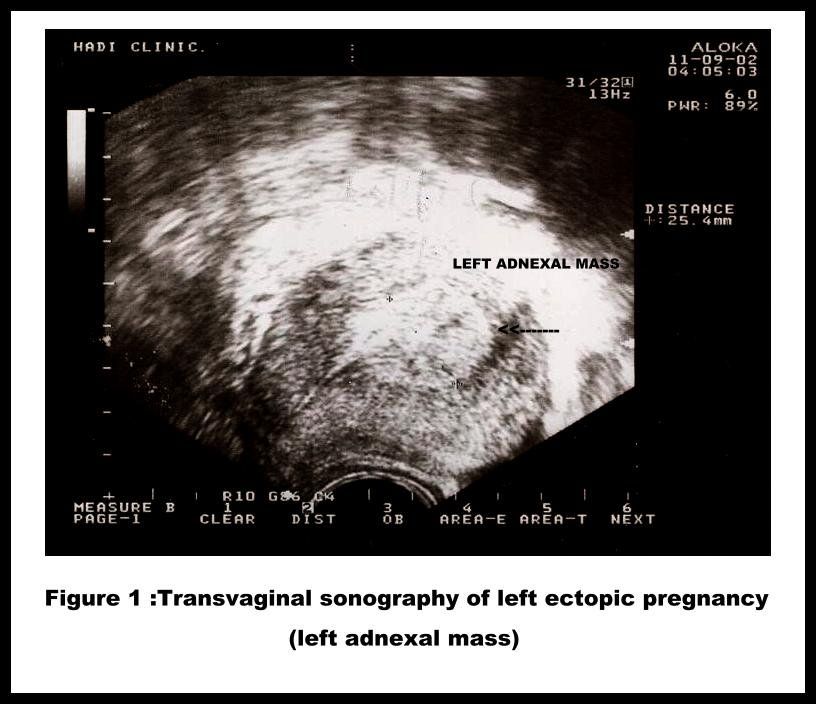
Method: In this prospective study there were 207 with a confirmed EP at Hadi Hospital and El-Rashed Hospital, private hospitals in Kuwait. Of these 184 were treated laparoscopically and 23 were treated by laparotomy. The diagnosis of EP was based on history, clinical symptoms, physical examination, a positive serum B-human chorionic gonadotrophin (B hCG), transvaginal ultrasonography and confirmed at laparoscopy. After surgery, to detect persistent viable trophoblastic tissue all patients were followed up by serial serum B-hCG levels on day 4 and day 7 and then weekly until non-pregnant levels (< 20 IU/l) were reached.
Results: Laparoscopic surgery gives an overall success rate of 98.9%. Linear salpingostomy was the main procedure performed in both groups. Estimated blood loss was significantly lower in the laparoscopy group (P<0.0001). The duration of operation in laparoscopy group was 66.46±19.97 min and 72.52±20.01 min in the laparotomy group. The duration of hospitalization was significantly shorter in the laparoscopy group (P<0.0001). Only 13 (7%) patients in the laparoscopy group required blood transfusion, whereas 6 (23%) in the laparotomy group needed transfusion (P<0.01). There were no intraoperative complications in either group. Eighty patients (47.3%) in the laparoscopy did not need analgesia after surgery compared to laparotomy group where all the patients need analgesia. The average time taken for the B-hCG to return to normal (<20 IU/l) was 12 days after conservative surgery in both groups. The cumulative frequency of hCG elimination down to the non pregnant level (<20 IU/l) was similar in both groups.
Conclusion: laparoscopic treatment (salpingostomy or salpingectomy) of EPs offers major benefits superior to laparotomy in terms of less blood loss, less need for blood transfusion, less need for postoperative analgesia and a shorter duration of hospital stay.
Keywords: laparoscopic surgery, ectopic pregnancy, laparoscopy, salpingostomy, salpingectomy.
Introduction and aim of work
The incidence of ectopic pregnancy (EP) has increased all over the world from 0.5% thirty years ago, to a present day 1-2%(1). This complication of early pregnancy, results in not only fetal loss, but also the potential for considerable maternal morbidity and the risk of maternal death (2)(3)(4). Until the risk factors that lead to EP are more fully understood, early detection and appropriate management will be the most effective means of reducing the morbidity and mortality associated with this condition (5)(6). Although the incidence of EP increased, with the improvement of diagnostic approaches, patients were detected at an earlier stage and possible to be treated more conservatively.(7). Surgery remains the mainstay of treatment.(8). Surgical treatments may be radical (salpingectomy) or conservative (usually salpingostomy), and they may be performed by laparoscopy or laparotomy (9). Improved anesthesia and cardiovascular monitoring, together with advanced laparoscopic surgical skills and experience, justifies operative laparoscopy for surgical treatment of EP even in women with hemodynamic instability.(10)(11). Improvements in management have led to a fall in the mortality rate from 2.9 per 1000 EPs in the early 1970s to 0.4 per 1000 in 1994-1996.(6).
This prospective clinical trial was conducted to compare the efficiency of laparoscopic treatment versus conventional abdominal surgery for tubal ectopic pregnancy and to review the clinical presentation, evaluate methods of diagnosis, and identifying the risk factors.
Patients and Methods
We conducted a prospective study in two centers: Department of Obstetrics and Gynecology, Hadi Hospital and Department of Obstetrics and Gynecology, El-Rashed Hospital, a private hospitals in Kuwait state, during the period from March 1999 to October 2001. During this period, there were 207 with a confirmed ectopic pregnancy (62 cases at El-Rashed hospital &145 cases at Hadi hospital). These patients were admitted through emergency or outpatient department. Patients were managed by laparoscopy (No 184) and by laparotomy (No 23).The diagnosis of ectopic pregnancy was based on history, clinical symptoms, physical examination, a positive serum B-human chorionic gonadotrophin (B hCG), transvaginal ultrasonography (ultrasound findings of empty uterus with or without adnexal mass), and confirmed at laparoscopy .All patients had diagnostic laparoscopy as the primary procedure to confirm the diagnosis and to evaluate the contra lateral tube before deciding which surgical approach would be performed. The selection of operative approach was not based on any defined criteria, but depended on the availability of laparoscopic facilities and the surgical team. Once the EP had been diagnosed laparoscopically, the choice of whether the patient would undergo a laparotomy or be managed laparoscopically depended on the surgeon on call. Those not trained in operative laparoscopy proceeded to perform a laparotomy. All laparoscopic procedures were performed by the first author at Hadi hospital and the second author at El-Rashed hospital. Patients were counseled pre operatively about the operative procedures and the risks and complications of operative laparoscopy, conservative procedures for EPs and the need for follow-up. All operations were conducted under general anesthesia with endotracheal intubation. After thorough evaluation, type of management was decided. Surgical procedure was performed and the surgical specimens were sent for histopathological examination. Ectopic pregnancy was histologically confirmed in all these specimens.
Operative laparoscopy
Laparoscopic surgery was performed using three ports. Following the establishment of pneumoperitoneum, a 10 mm 00 laparoscope was introduced through an 11 mm cannula in intra-umbilical incision. After a confirmation of the diagnosis and laparoscopic treatment was deemed possible, a 5 mm puncture was made in the left and right lower quadrant using direct visualization and transillumination to avoid the epigastric vessels with continuous high flow carbon dioxide insufflators. The procedure was visualized on a video monitor using a camera (Endovision Telecam, Karl Storz, Germany) attached to the eyepiece of the telescope. Linear salpingostomy was performed by making a linear incision in the anti mesenteric border of the affected tube over the tubal swelling with point needle monopolar diathermy. The pregnancy was removed with a forceps, the tube was irrigated with lactated Ringer's solution and haemostasis was achieved with bipolar diathermy. The tubal incision was then left to heal by secondary intention. Laparoscopic total salpingectomy was performed by progressive coagulation and cutting of the mesosalpinx, starting with the fimbriated end and progressing to the proximal isthmic portion of the tube. There, it was separated from the uterus after bipolar coagulation or loop-type ligation and cutting with scissors. Milking of tube (tubal expression) was done for patients with fimbrial EP. The pregnancy was removed from the abdominal cavity via a 10 mm port.
Just prior to withdrawal of the laparoscope the pneumoperitoneum was released and haemostasis was checked to ensure that any 'tamponade effect' caused by the raised intra abdominal pressure was detected. The pelvis was irrigated with copious amounts of lactated Ringer's solution until all blood clots were evacuated. Adhesions in the contra lateral fallopian tube were freed, if present. Half litre of lactated Ringer's solution was left in the pelvis at the conclusion of the operation to help prevent adhesion formation (12). In the presence of haemoperitoneum, the amount of blood present was assessed by the difference between the amounts of fluid irrigated and evacuated. Post-operative management followed the normal practice in both departments. Analgesia was prescribed to the patients on demand, namely pethidine, 1.5 mg/kg IM every four hours or diclofenac sodium 100 mg, (Rofenac tablets & ampoules, Spimaco, Saudi Arabia). An outpatient follow up appointment was arranged for four to six weeks after discharge from hospital.
Laparotomy
Laparotomy was performed through a Pfannenstiel incision and standard surgical techniques (the same laparoscopic techniques were applied). After surgery, To detect persistent viable trophoblastic tissue all patients were followed up by serial serum B-hCG levels on day 4 and day 7 and then weekly until non-pregnant levels (< 20 IU/l) were reached, with weekly clinical examination and transvaginal ultrasound scans if needed.
Statistical evaluation
The clinical and surgical data were recorded in an investigative report form. These data were transferred to IBM-card, using IBM-PC with statistical program SPSS under window VER.6.1 to obtain: 1-Descriptive Statistics: A-Mean, B-Standard deviation (±S.D), C-Range (minimum-maximum), D-Number and percent .2-Analysis Statistics: a Student’s ? t test, Chi square test and Fisher’s exact test. P-value of less than 0.05was considered significant.
Results
During the study period, 207 patients presented with an EP (all of these were included in the study) and 19060 live births (7260 at El-Rashed hospital & 11800 at Hadi hospital) giving a total incidence of 1 ectopic pregnancy for every 92 (1.1%) live births. Patients were divided into 2 groups: Group I (n=184) had their EPs removed laparoscopically; Group II (n=23) had a laparotomy. A comparison of the demographic and clinical data of the two groups is shown in Table 1. There were no difference in the mean age, parity, preoperative serum B-hCG, past gynecological history of pelvic infection, frequency of previous EP, prior laparotomy, gestational age at the time of surgery, use of intrauterine device and preoperative hemoglobin levels. Most (58%) of our patients were within the 21-32 age group. Parous women constituted 64% and nulliparous patients constituted 23% of the study group. previous history of abortion was found in 26% of the patients. According to the ethnicity of women included in the present study, they were:1:Kuwaitis (175 women), 2:Non-Kuwaitis,other Arabs (14 women), 3:Non-Kuwaiti, Non-Arab (18 women). The diagnosis of EP was based on history, clinical symptoms, physical examination, a positive serum pregnancy test, transvaginal sonography and laparoscopy. History of infertility was found in 14%,Use of an intrauterine contraceptive device was found in 12% and Previous ectopic pregnancy was found in 3.4%.The presenting symptoms were abdominal pain (96%), short period of amenorrhea (89%) and Vaginal bleeding (79%).The presenting signs were abdominal tenderness (89%),and adnexal tenderness (64%). The diagnoses of EP in 86% were confirmed by ultrasound. The study showed that 40% of EP was ruptured at the time of presentation.
The operative outcome is summarized in table 2. All the EPs were tubal. In 164 patients (79.2%) it was in the right fallopian tube and in 43 patients (20.8%) it was in the left fallopian tube. Among those attempted laparoscopically, only two had to undergo a laparotomy because of failure of the laparoscopic approach. This gives an overall success rate of 98.9% for attempted laparoscopic removal of the pregnancy. Failure of the laparoscopic approach because in one case it was not possible to achieve pneumoperitoneum because of extreme obesity. In the second case because of technical problems in the instruments. There was no difference in the mean diameter of the intact tubal pregnancy. The incidence of haemoperitoneum (>100 ml of blood in the pelvis) was lower in the laparotomy group. The greatest estimated haemoperitoneum was 2,340 mL. Estimated blood loss was significantly lower in the laparoscopy group (P<0.0001). Linear salpingostomy was the main procedure performed in the laparoscopy and laparotomy groups (96.2% &73.9% respectively) (table 2).
The duration of operation in laparoscopy group was 66.46±19.97 min and 72.52±20.01 min in the laparotomy group and the difference between the durations of operations was not considered to be significant. The duration of hospitalization was significantly shorter in the laparoscopy group (P<0.0001). Only 13 (7%) patients in the laparoscopy group required blood transfusion, whereas 6 (23%) in the laparotomy group needed transfusion (P<0.01). There were no intraoperative complications in either group. Postoperatively four patients in the laparoscopy group developed bruising over the umbilical wound, which resolved spontaneously with ordinary care, while one patient in the same group developed extensive bruising over the umbilical wound and extended to the lower abdomen, which resolved after three weeks with ordinary care. Eighty patients (47.3%) in the laparoscopy did not need analgesia after surgery compared to laparotomy group where all the patients need analgesia.
On analysis of the pathological changes of ectopic trophoblastic tissue it was found that 113 (54.59%) specimens were histologically reported as unremarkable deciduas and chorionic villi, 39 specimens (18.84%) as hemorrhage with degenerated product of conception,28 (13.53%) as trophoblastic tissue with hemorrhage, and 27 (13%) as trophoblastic tissue with fibrosis. The average time taken for the B-hCG to return to normal (<20 IU/l) was 12 days after conservative surgery in both groups. The cumulative frequency of hCG elimination down to the non pregnant level (<20 IU/l) was similar in both groups (Fig 1).
Discussion
The technical advancement in the field of minimal access surgery has greatly enhanced the possibility of both diagnosing and treating EP effectively. (13). Since the first excision of a tubal pregnancy through a laparoscope by Shapiro & Adler (14), it has been used with increasing frequency. and the laparoscopic approach for management of EP has replaced laparotomy. (8)(15). The frequency of EP in our series was 1.1%.In Abha, Saudi Arabia the incidence of EP was 0.74 per 100 live births (16). In northern Europe between 1976 and 1993 the incidence increased from 11.2 to 18.8 per 1000 pregnancies. (17). In the United Kingdom there are around 11 000 cases of EP per year (incidence 11.5 per 1000 pregnancies) (18). Although the present study has not focused on the risk factors of EPs many such well factors have been reported in literature (19)(20). The predisposing factors, which have been demonstrated in the present study, were almost comparable with those found in a previous studies.(20)(21). The presence of known risk factors can increase suspicion, but any sexually active woman presenting with abdominal pain and vaginal bleeding after an interval of amenorrhea has an EP until proved otherwise (8). In the present study The most important symptoms were abdominal pain (96%), short period of amenorrhea (89.1%) and vaginal bleeding (79%). These were comparable with other studies. (22) The study also demonstrated that the most important signs were abdominal tenderness (89%) and adnexal tenderness (64%). History and physical examination alone do not reliably diagnose or exclude EP, as up to 9% of women report no pain and 36% lack adnexal tenderness (8). The usefulness of ultrasound in the study was confirmed by the fact that 86% were confirmed by ultrasound (fig 2). The presence of an intrauterine pregnancy generally excludes EP, although other ultrasound findings have to be considered, especially if symptoms are atypical, severe, or persistent. The use of quantitative measurement of serum concentrations of B hCG together with transvaginal ultrasonography has improved the diagnosis of EP. (23)
The study showed that 40% of EPs were ruptured at the time of presentation. In the prospective study of Soyannwo the ruptured EPs were 81.1%.(24). This difference may be related to the fact that most Kuwaiti women are regularly attendants for antenatal care starting in very early pregnancy and they are keen to do early B hCG and transvaginal sonography. In our laparoscopic group, the greatest estimated hemoperitoneum was 2,340 mL and the procedure was carried through successfully. Laparoscopy is not only suitable for early EPs but it is also safe and feasible in instances where there is tubal rupture and hemoperitoneum, provided the patient is not severely compromised haemodynamically (25) (26) There was a significant reduction of total blood loss (P<0.0001), number of patients who needed blood transfusion (P<0.01), total days needed for hospital admission (P<0.0001) and the need for postoperative analgesia in the laparoscopic group versus laparotomy group (P<0.0001). These findings were in agreement with previous studies. (9)(27)(28). In the present study laparoscopic techniques (salpingostomy or salpingectomy) do not increase the operating time. In fact, it actually saves time, as during a laparotomy, opening and closing the abdomen just to gain access to the affected tube consumes precious operating time. Previous comparative studies support this (9) (29). In the present study we have demonstrated that EPs can be managed successfully via minimal access surgery and Laparoscopic management offer several advantages over conventional treatment via laparotomy (table 2). It not only results in reduced hospital stay with associated financial savings but also reduced patient morbidity, enabling women to return to their normal activities much sooner.(9)(19)(26). Also it has been shown that conservative surgery is more likely to be performed if the laparoscopic approach is used.(26). Our study confirms these results. The laparoscopic procedure performed depends on the site of the EP. An ampullary pregnancy is best be dealt with by performing a linear salpingostomy as described above. Linear salpingostomies are allowed to heal by secondary intention as it has been shown that there is no significant difference in adhesion formation nor in tubal patency rates whether the tube is sutured or not and the cumulative intra uterine pregnancy rates are similar (30). Cornual pregnancies generally require a laparotomy and surgical excision (31); although cases have been successfully managed via the laparoscope (32).
Our study confirm this. If the affected tube is conserved, the patient should be followed by serial hCG estimations until these return to normal. This can take several weeks and the patient should be made aware of that possibility pre-operatively. Follow up is necessary because of the possibility of persistent trophoblastic tissue in the fallopian tube. Most series report an incidence of 5-10 %.(26) (33). We had no cases amongst the 201 patients who had conservative surgery on the tubes (in both groups), with persistent trophoblastic tissues after surgery. These findings may be due to the preoperative levels of serum b-hCG < 3000 IU/l. Brumsted et al. (29) reported a frequency of second interventions of 8% in their laparoscopy group and zero in their laparotomy group. Complication in terms of second surgical intervention are related to the preoperative levels of serum hCG (34). In our study the postoperative elimination of hCG was similar in both the laparoscopy and laparotomy-treated patients, whether treated by conservative salpingostomy or radical salpingectomy, implying that the radicality in removing the trophoblastic tissue is as efficient by laparoscopy as by laparotomy. In the present study we have demonstrated that, the majority of tubal ectopic pregnancies can be managed laparoscopically. During the study period, of the 186 patients in whom laparoscopic management was attempted, 98.9% were successful. Operative laparoscopy is currently the best treatment for EP (8).The benefits to patients are self-evident and our findings are supported in the literature.
We concluded that laparoscopic treatment (salpingostomy or salpingectomy) of EPs offers major benefits superior to laparotomy in terms of less blood loss, less need for blood transfusion, less need for postoperative analgesia and a shorter duration of hospital stay.
Table 1

Table 2
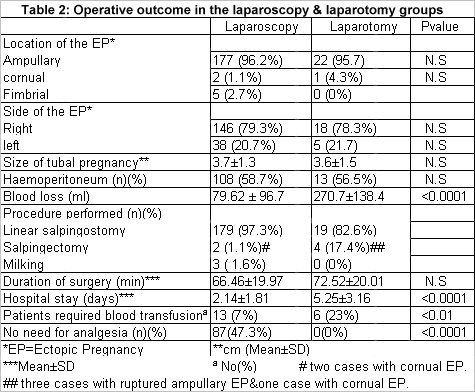
Figure 1

Figure 2
References:
References
1. Lehner R, Kucera E, Jirecek S, Egarter C, Husslein P. Ectopic pregnancy. Arch Gynecol Obstet 2000 Feb;263(3):87-92
2. Centres for disease control (CDC).Ectopic pregnancy -- United States, 1988-1989. MMWR 1992; 41:591-4.
3. Centres for disease control (CDC).Ectopic Pregnancies - United States, 1990-1992. MMWR 1995; 44:46-48.
4. Why women die. Report on confidential enquiries into maternal deaths in the United Kingdom 1994-1996. Norwich: Stationery Office, 1998.
5. Leach RE, Ory SJ. Management of ectopic pregnancy. Am Fam Physician 1990; 41:1215-22.
6. Ory SJ. New options for diagnosis and treatment of ectopic pregnancy. JAMA 1992;267:534-7.
7. Feng W, Cao B, Li Q. Advances in diagnosis and treatment of ectopic pregnancy during the past ten years. Zhonghua Fu Chan Ke Za Zhi 2000 Jul;35(7):408-10 (abstract).
8. Tay J I , Moore J,Walker J J. Ectopic pregnancy: Clinical review BMJ 2000;320(1):916-919.
9. Murphy AA,Nager CW,Wujek JJ,Kettel JM,Torp VA,Chin HG.Operative laparoscopy versus laparotomy for the management of ectopic pregnancy: a prospective trial.Fertil Steril 1992;57:1180-5.
10. Sagiv R, Debby A, Sadan O, Malinger G, Glezerman M, Golan A. Laparoscopic surgery for extrauterine pregnancy in hemodynamically unstable patients. J Am Assoc Gynecol Laparosc 2001 Nov;8(4):529-32.
11. Chapron C, Fernandez H, Dubuisson JB. Treatment of ectopic pregnancy in 2000. J Gynecol Obstet Biol Reprod (Paris) 2000 Jun;29(4):351-61.
12. Younis MN,Hamed AF,El Tabbakh MN.Effect of antiprostaglandindins,corticosteroids and anticoagulants for prevention of postoperative adhesions after tubal surgery. Paper presented in the third world conference in Fallopian tube in health and disease,1990;July 3-6,Kiel, Germany.
13. Ghosh S, Mann C, Khan K, Gupta JK. Laparoscopic management of ectopic pregnancy. Semin Laparosc Surg 1999 Jun;6(2):68-72.
14. Shapiro HL, Adler DH. Excision of an ectopic pregnancy through the laparoscope. Am J Obstet Gynaecol 1973; 117:290.
15. Vasile C, Litta P, Sacco G, Minante M.Laparoscopic surgical approach to ectopic pregnancy. Clin Exp Obstet Gynecol 1999;26(1):35-8.
16. Eric I. Archibong, Adekunle A. Sobande. Ectopic pregnancy in Abha, Saudi Arabia. A continuing conundrum. Saudi Medical Journal 2000; Vol. 21(4): 330-334
17. Storeide O, Veholmen M, Eide M, Bergsjo P, Sandevi R. The incidence of ectopic pregnancy in Horlaland County, Norway 1976-1993. Acta Obstet Gynecol Scand 1997; 76: 345-349
18. Why women die. Report on confidential enquiries into maternal deaths in the United Kingdom 1994-1996. Norwich: Stationery Office, 1998.
19. Vermesh M. Conservative management of ectopic gestation. Fertil Steril 1989;51:559-67.
20. Pisarska MD, Carson SA, Buster JE. Ectopic pregnancy. Lancet 1998; 351: 1115-1120
21. Mitchell DE, McSwain HF, McCarthy JA, Peterson HB. Hysterosalpingographic evaluation of tubal patency after ectopic pregnancy. Am J Obstet Gynecol 1987; 157: 618-622.
22. Leach RE, Ory SJ. Modern management of ectopic pregnancy. J Reprod Med 1989; 34: 324-338.
23. Ankum WM, Hajenius PJ, Schrevel LS, van der Veen F. Management of suspected ectopic pregnancy. Impact of new diagnostic tool in 686 consecutive cases. J Reprod Med 1996; 41: 724-728
24. Soyannwo OA. Ectopic pregnancy and anesthesia in Gambia. Int J Gynaecol Obstet 1994; 46: 331-332.
25. Maruri F, Azziz R. Laparoscopic surgery for ectopic pregnancies: technology assessment and public health implications. Fertil Steril 1993; 59:487.
26. Baumann R, Magos AL, Turnbull A. Prospective comparison of videopelviscopy with laparotomy for ectopic pregnancy. Br J Obstet Gynaecol 1991; 98:765.
27. Lundorff P, Thorburn J, Lindblom B. Fertility outcome after conservative surgical treatment of ectopic pregnancy evaluated in a randomized trial. Fertil Steril 1992; 57: 998-1002.
28. Vermesh M, Silva PD, Rosen GF, Stein AL, Fossum GT, Sauer MV. Management of unruptured ectopic gestation by linear salpingostomy: A prospective, randomized clinical trial of laparoscopy versus laparotomy. Obstet Gynecol 1989; 73: 400-403.
29. Brumsted J,Kessler C,Gibson C,Nakajima S,Riddick DH,Gibson M.A comparison of laparoscopy and laparotomy for the treatment of ectopic pregnancy.Obstet Gynecol 1988;71:889-92.
30. Hill GA, Sigars J, Sigars JR, Herbert III CM. Laparoscopic management of interstitial pregnancy. J Gynaecol Surg 1989;5:209-212.
31. Tulandi T, Guralnick M. Treatment of tubal ectopic pregnancy by salpingotomy with or without tubal suturing and salpingectomy. Fertil Steril 1991;55:53-55.
32. Reich H, McGlynn F, Brudin R, Tsontsoplides G, De Caprio J. Laparoscopic treatment of ruptured interstitial pregnancy. J Gynaecol Surg 1990;6:135-138.
33. Donnez J, Nisolle M. Laparoscopic treatment of ampullary tubal pregnancy. J Gynaecol Surg 1989;5:19-24.
34. Lundorff P,Hahlin M,Thorburn J,Kallfelt B,Lindblom B.Laparoscopic surgery versus conventional conservative surgery for tubal pregnancy.Presented at the Second World Congress of Gynecologic Endoscopy,June 5-8,1998,Clermont-Ferrand,France.
Reducing multifetal pregnancy through publicly funded IVF programs
April 26th 2024Learn how a mandatory elective single-embryo transfer policy in publicly funded in vitro fertilization programs significantly decreases multifetal pregnancy rates, offering insights into mitigating risks in assisted reproduction.
Read More
Recap on reproductive rights with David Hackney, MD, MS
December 20th 2022In this episode of Pap Talk, we spoke with David Hackney, MD, MS, maternal-fetal medicine physician at Case Western Reserve University and chair of ACOG's Ohio chapter for a full recap of where restrictions on reproductive rights have been and where they're going.
Listen
In this episode of Pap Talk, Gloria Bachmann, MD, MSc, breaks down what it means to be a health care provider for incarcerated individuals, and explores the specific challenges women and their providers face during and after incarceration. Joined by sexual health expert Michael Krychman, MD, Bachmann also discusses trauma-informed care and how providers can get informed.
Listen
Unlocking placenta accreta spectrum with single-cell gene targets
April 18th 2024Discover how cutting-edge single-cell RNA sequencing unveils molecular insights into placenta accreta spectrum disorders, potentially revolutionizing diagnostics and treatments for this life-threatening pregnancy complication.
Read More
