Laparoscopic Procedures
Laparoscopy is now an option for many gynecological conditions. This overview discusses specific laparoscopic procedures and the conditions they treat.
Laparoscopic and Minimally Invasive Procedures
- Laparoscopic assisted Vaginal Hysterectomy (LAVH)
- Paravaginal Repair (Cystocele Repair)
- Burch Repair (Incontinence Surgery)
- Paravaginal Plus Burch urethropexy
- Laparoscopic Uterine Suspension
- Enterocele Repair
- Vaginal Vault Suspension (Support Vaginal Apex)
- Salpingo-oopherectomy (Removal of Fallopian Tubes and Ovary)
- Adhesiolysis
- Fistula repair
Laparoscopic Assisted Vaginal Hysterectomy
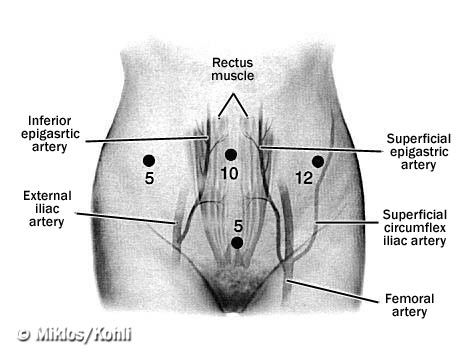
Hysterectomy is the surgical removal of the uterus. This is one of the most commonly performed gynecologic surgeries in the United States. Almost 750,000 women undergo hysterectomy each year. Though there are three major approaches to uterine removal, the most commonly performed approach is through a large abdominal incision (aka abdominal hysterectomy). Other approaches include the vaginal hysterectomy and the laparoscopic assisted vaginal hysterectomy. The vaginal hysterectomy is less morbid with no abdominal incision and patients recover more quickly postoperatively. However, when patients have abdominal pain, vaginal prolapse, urinary incontinence, or adhesive disease, a laparoscopic approach to hysterectomy is the most beneficial way of removing the uterus while addressing any of the above problems. In other words, the greatest benefit is the potential to convert what would have been an abdominal (laparotomy) incision to mini incisions. Benefits of a laparoscopic assisted vaginal hysterectomy:
- Miniature abdominal incisions
- Access to cut any painful adhesions
- Access to perform oopherectomy
- Access to perform vaginal vault suspension
- Access to perform Burch urethropexy
- Access to perform paravaginal repair
- Excellent exposure
- Quicker recovery time
Laparoscopic Paravaginal Repair (cystocele repair)
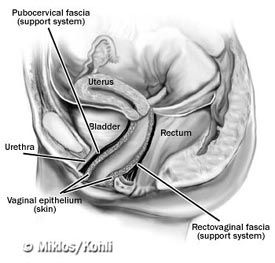
The bladder and urethra are supported by the anterior or upper vaginal wall. When there is a break in the support of the anterior vaginal wall, the bladder and urethra fall, resulting in a cystourethrocele. Review of the gynecologic literature reveals that the most common reason for so called "bladder drop" is a paravaginal defect or loss of support of the lateral attachment of the vagina. Greater than 90% of cystoceles are due to paravaginal defects. In an attempt to repair the cystocele, most physicians would perform an anterior repair (anterior colporrhaphy) however, this is rarely the correct anatomical operation. In patients with paravaginal defects, the most appropriate surgical procedure is the paravaginal repair.
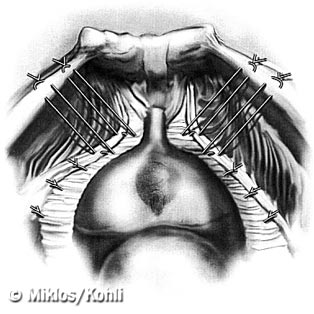
The paravaginal repair is accomplished by suturing the lateral aspect of the anterior vaginal wall back to its original point of attachment known as the arcus tendineus fascia pelvis (ATFP) or the "white line". Re-approximation of the vaginal wall to the fascia overlying the obturator internus muscle will restore the bladder and the urethra to its normal anatomical position. Important points of paravaginal repair:
- 90% of cystoceles are due to paravaginal defects
- Paravaginal repairs are traditionally performed using sutures
- Paravaginal and mid-line defects can be present simultaneously
- Paravaginal repairs can be performed laparoscopically
- Paravaginal repairs can be performed with Burch urethropexy (incontinence)
- Paravaginal repairs can be coupled with other prolapse surgeries
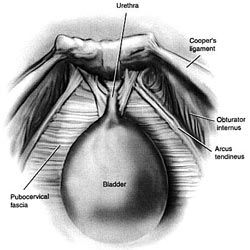
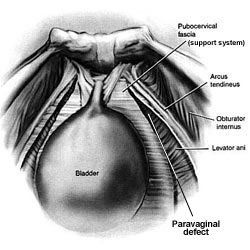
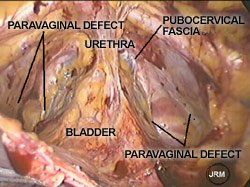
Paravaginal defects - Loss of lateral vagina attachment at the arcus tendineus resulting in a cystocele (bladder drop).
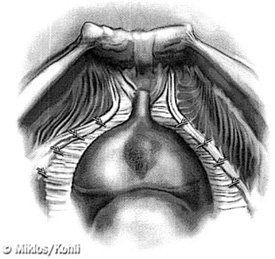
Paravaginal Defect Repair - Repairing the vagina restores support to the bladder thus removing the cystocele or bladder drop.
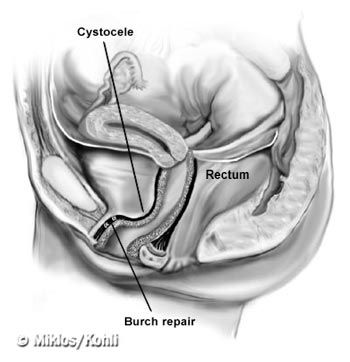
Laparoscopic Burch Urethropexy
Since the introduction of the urethral suspension procedure in 1910, over 100 different surgical techniques for the treatment of genuine stress urinary incontinence have been described. Recently the AUA, American Urology Association, has confirmed that the two most curative and enduring operations are the Burch urethropexy and the pubovaginal sling. The Burch procedure was introduced by John Burch, MD in 1961 and has remained an outstanding operation for the treatment of activity related urinary incontinence. Emphasizing the principles of minimally invasive surgery, the laparoscopic approach has been successfully adopted for the Burch procedure. The Burch procedure should be performed in the exact same manner as if it were being performed through a large abdominal incision. Burch urethropexy facts:
- can be performed laparoscopically
- can be performed via laparotomy
- cure rate of 85% --5-10 years after the operation
- can be combined with other prolapse surgeries
- has minimal morbidity
REVIEW OF THE SURGICAL LITERATURE - LAPAROSCOPIC BURCH
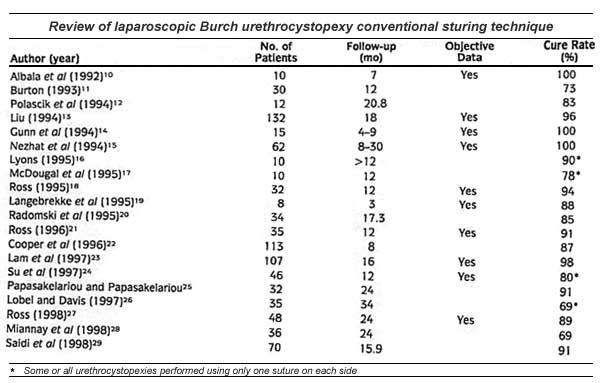
Most recent published literature describes the Burch urethropexy utilizing:
- Four permanent sutures
- Two sutures are placed at the level of the midurethra
- Two sutures are placed at the level of the bladder neck
- All sutures are passed through the Coopers ligament
- Higher cure rates utilizing four sutures instead of two sutures
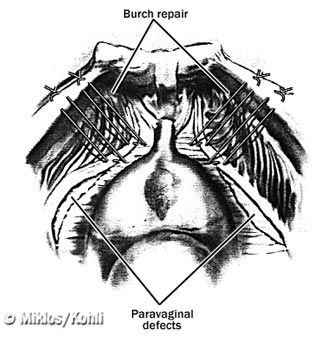
Laparoscopic "Paravaginal Plus Burch" Urethropexy
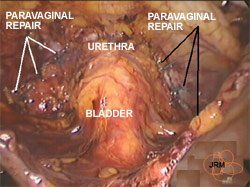
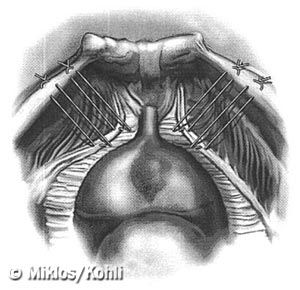
Dr. Miklos' recent study review of the more than 200 patients who had received a laparoscopic Burch urethropexy revealed more than 90% of these patients also required a paravaginal repair. Dr. Miklos previously described combining these two surgical techniques in an attempt at restoring anterior vaginal wall anatomy and correcting the stress urinary incontinence. This surgical procedure is recommended for patients with cystocele (due to paravaginal defects) and stress urinary incontinence. The paravaginal repair is performed between the apex (highest point) of the anterior vaginal wall and the "bladder neck" (urethra meets the bladder) this part of the surgery corrects the cystocele (bladder drop). The Burch urethropexy is performed to stabilize and support the urethra. The combined surgical procedure routinely utilizes:
- Total of ten sutures
- Six sutures for the paravaginal repair (cystocele repair)
- Four sutures for the Burch urethropexy (incontinence repair)
- All permanent sutures
Side View of Anterior Vaginal Wall Prolapse and Repair.
Laparoscopic Uterine Suspension
Traditional medicine recommends removal of the uterus when there is uterine prolapse. In cases of severe uterine and vaginal prolapse a hysterectomy followed by vaginal wall reconstruction may still be the most beneficial therapy. However there are more women who are electing to keep their uterus especially in those whom the uterus is only mildly or moderately prolapsed. The decision to attempt uterine and vaginal support is made only after a full informed consent is made with the patient having the operation. One of the most important aspects of this surgery is the lack of long term data supporting its utilization in uterine and vaginal prolapse surgery.
Dr. Miklos will perform laparoscopic uterine suspension surgery in selected patients. The uterine support surgery that he performs is based upon restoration of the normal supportive endopelvic fascia. Dr. Miklos has never performed a uterine suspension surgery without correcting other vaginal prolapse defects present. It is Dr. Miklos' experience that anyone having a uterine suspension will most likely need a paravaginal repair, possibly a posterior repair and or Burch procedure.
There are many methods of uterine suspension including sacrospinous ligament suspension, abdominal sacral colpopexy (mesh between uterus and tailbone) and uterosacral ligament suspension. Dr. Miklos routinely performs the laparoscopic approach to uterosacral ligament suspension.
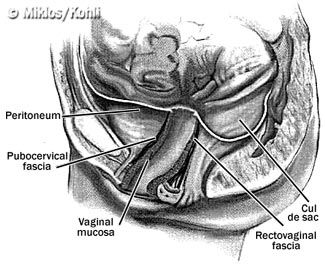
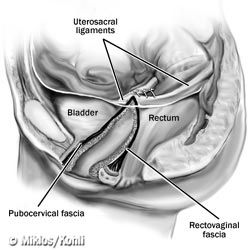
Enterocele Repair
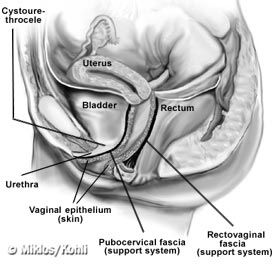
Enterocele formation usually occurs in women who have had a hysterectomy. Most reconstructive surgeons believe this is in part due to the removal of the uterus. To understand the repair of an enterocele one must first understand the anatomy of this defect. An enterocele is defined as peritoneum (skin on the inside of the abdominal cavity) in direct contact with vaginal epithelium (skin of the vagina) with no intervening fascia (support structure). To repair this defect or hernia, the supportive structure must be reconstructed. The support structure at the apex of the vagina is the pubocervical fascia (anterior vaginal wall) and the rectovaginal fascia (posterior vaginal wall). The apex of both vaginal walls usually fuses into the uterus. However, inpatients where the uterus has
been removed (hysterectomy), sometimes the supportive layers of the anterior and posterior walls have not fused or scarred together, leaving an area lacking support. Therefore a herniation at the apex of vagina allows the peritoneum to come in direct contact with vaginal skin and create a bulge.
Repair of the defect involves suturing the apex of pubocervical and rectovagina fascia back together. These sutures will only repair the apical defect; it will not support the apex of the vagina to a supporting structure. Usually patients receiving an enterocele repair also require a vaginal apex suspension (vaginal vault suspension).
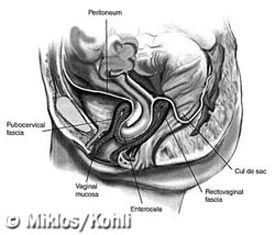
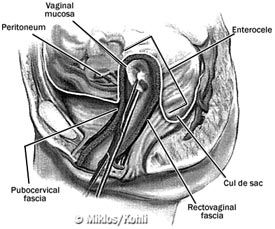
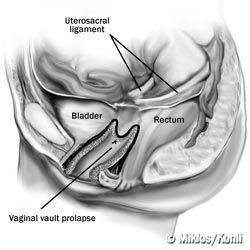
Enterocele - defect in the pubocervical fascia and rectovaginal fascia. The second picture shows the elevation of the defect into the abdominal cavity.
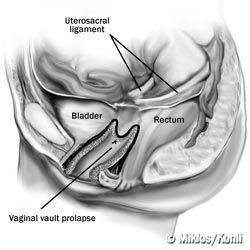
Vaginal Vault Suspension
As described earlier, a vaginal vault prolapse means the apex of the vagina (upper 20-30% of the vagina) has broken away from its original support structure known as the uterosacral ligaments. The uterosacral ligaments hold up the apex and the uterus when the uterus is in place. When the uterus is removed (hysterectomy) the uterosacral ligaments must be cut to remove the uterus. In an attempt at preventing future vaginal apex or vault prolapse the uterosacral ligaments should be attached to the apex of the vagina before removing the patient from the operating room.
If the patient did not have her uterosacral ligament attached to the vaginal apex or the uterosacral ligaments did not remain attached after the surgery, the patient risks ending up with vaginal vault prolapse. As the prolapse continues to pull down, it will increase the risk of anterior and posterior paravaginal defects.
There are many ways to perform vaginal vault suspension. Three commonly described methods are:
- sacrospinous ligament suspension
- abdominal sacral colpopexy (mesh between vagina and tailbone)
- uterosacral ligament suspension (restore normal anatomy)
Dr. Miklos has expertise performing all three operations but prefers a laparoscopic approach to uterosacral ligament suspension. This entails suturing the uterosacral ligament to the apex of the vagina. This procedure is normally performed by placing two sutures through each uterosacral ligament and then through the cuff or apex of the vagina. The suture is tied to support the cuff or apex to the uterosacral ligaments. This operation is very similar to the uterine suspension procedure above except the uterus is not in place. Most patients requiring a vaginal vault suspension also require other reconstructive supportive procedures such as:
- paravaginal repair
- enterocele repair
- posterior repair
- Burch urethropexy
Salpingo-oopherectomy
Salpingo--oophorectomy is the surgical removal of the ovary and the fallopian tubes. The procedure is often performed at the time of hysterectomy. Some common reasons for this
surgery include:
- Ovarian cysts
- Endometriosis
- Recurrent pelvic pain
- Postmenopausal
This procedure can also be performed laparoscopically. Adhesions or scar tissue, which are usually involved, can make this procedure difficult and complicated and in the past required a large abdominal incision. However, gynecologists skilled in laparoscopic surgery have perfected this technique. Patients who require only this procedure often are able to go home the same day as surgery.
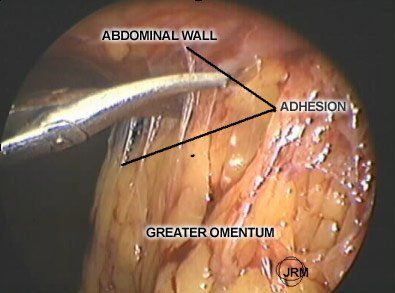
Adhesiolysis
Adhesiolysis is the surgical removal or take down of scar tissue within the abdominal cavity. Patients more likely to have adhesive disease:
- Previous pelvic or abdominal surgery
- History of peritonitis (infection of the abdominal cavity)
- History of radiation therapy
- Previous intrabdominal trauma or bleeding
Patients with intra-abdominal adhesive disease may experience:
- Pelvic or abdominal pain/discomfort
- Abnormal bowel habits
- Bowel obstruction
- Bloating
- Constipation
Adhesiolysis can be performed laparoscopically or through a laparotomy. The goal of adhesiolysis is to surgically remove or take down the adhesions. Many surgeons use laser, electroenergy or electrocoagulation to perform this procedure. Dr. Miklos performs these procedures using scissors, just like he would do if he did the surgery through an open large incision. Dr. Miklos believes that laparoscopy is only a mode of access into the abdominal cavity and should not change the way one performs an operation. Most patients having an adhesiolysis performed usually remain in the hospital for 23 hours and released.
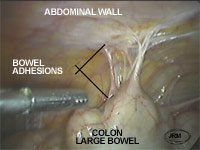
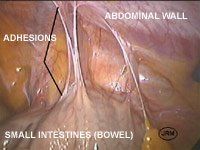
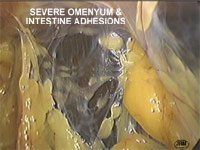
Abdominal adhesions - Three different patients with adhesions inside the abdominal cavity. Adhesions can come in various sizes, length and structure. No matter what the size they can cause abdominal pain, discomfort, bloating, and difficulty with bowel movements.
Fistula repair
Vesicovaginal (bladder and vaginal) fistula repairs are most commonly performed via the vagina. However, on occasion patients fail after a vaginal attempt at surgical correction. In that situation or in fistula that appear very high up or towards the apex of the vagina, a laparoscopic approach is sometimes beneficial. Dr. Miklos has published some of the first laparoscopic repair of bladder vaginal and uterine vaginal fistula in the scientific literature.
Copyright ©2000, 2001 Dr. John R. Miklos
All text and images in this article are property of Dr. John R. Miklos and may not be reproduced in any way without permission
Unlocking placenta accreta spectrum with single-cell gene targets
April 18th 2024Discover how cutting-edge single-cell RNA sequencing unveils molecular insights into placenta accreta spectrum disorders, potentially revolutionizing diagnostics and treatments for this life-threatening pregnancy complication.
Read More
Excessive gonadotropins in IVF: Effects on mosaicism and live birth
April 12th 2024A recent study revealed a correlation between high doses and prolonged duration of exogenous gonadotropin use during in vitro fertilization and increased embryonic mosaicism alongside diminished live birth rates, prompting reconsideration of dosage and duration protocols.
Read More
