Case Study: Characteristics of Fetal Hiatal Hernia
Figure 1. Courtesy of Durr-e-Sabih, MBBS, MSc, FRCP (click to enlarge).

Figure 2. Courtesy of Durr-e-Sabih, MBBS, MSc, FRCP.
A 28-year-old woman, 17 weeks pregnant with her first child, presented for a routine obstetrical ultrasound to rule out congenital fetal anomalies.
History: This patient had normal menstrual cycles prior to the pregnancy. She had no history of diabetes mellitus, hypertension, or any other major illnesses and reported having one sibling.
Present pregnancy: A 17-week history of amenorrhea corresponds with the age of the fetus on ultrasound scan. No discharge or abdominal pain during this pregnancy was reported.
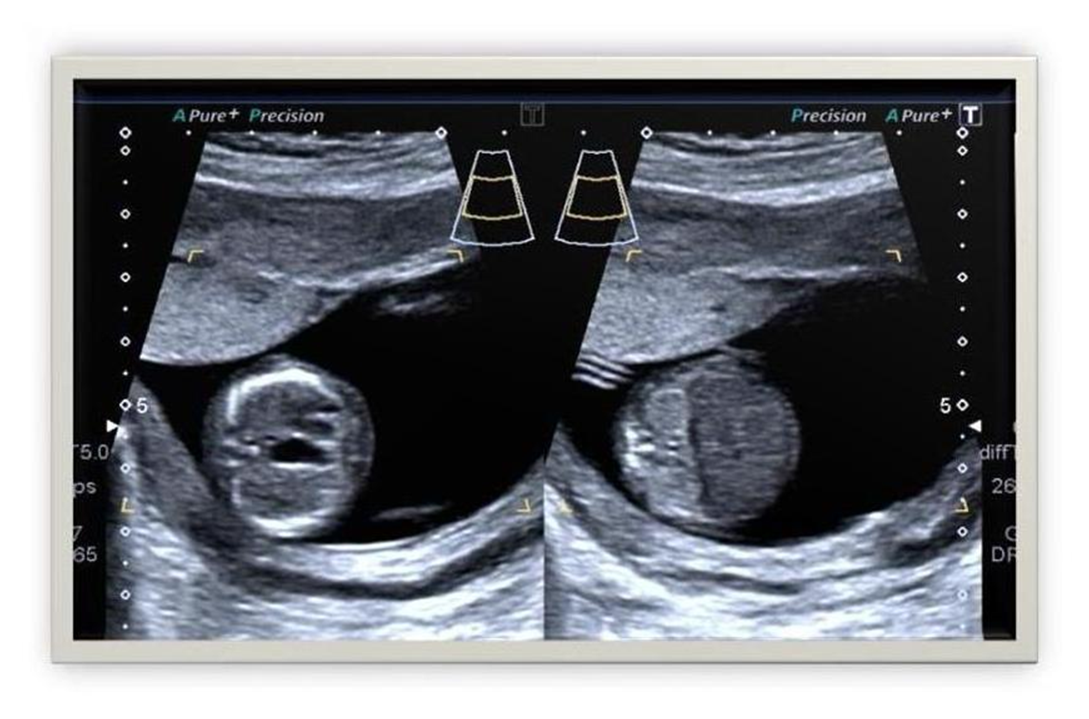
Imaging studies: This patient underwent routine transabdominal ultrasonography to exclude any congenital fetal anomalies. She had not undergone any previous ultrasound scan. The B-mode images of this examination are shown in Figure 1 and Figure 2.
Physical examination: Blood pressure was normal at 122/78 mm Hg. Other vital signs were within normal limits, and no abnormalities were noted on chest examination. On abdominal examination, the fundal height of the patient matched the gestational age of 17 weeks.
What are your findings based on these images?
Sonographic Findings
Figure 1 shows a transverse section of the fetal chest and abdomen. The placenta appears to be anterior and grossly normal, as does the amniotic fluid level in the uterine cavity. However, there is an anechoic lesion in the fetal thorax.
The oval-shaped anechoic lesion appears to be well within the thoracic cage and located posterior to the fetal heart. Could the lesion be coming from the fetal heart or the fetal lungs? A closer look at Figure 2 shows a fetal heart and fetal lungs that appear grossly normal. The lesion appears to be in the midline, which could suggest it arises from the fetal aorta or inferior vena cava. However, the lesion is separate from both these vessels. The spine may be the source of the lesion, but the lesion is too far anterior to the fetal thoracic spine. Could it be the fetal kidneys? The kidneys are markedly hyperechoic, but is this an incidental finding or related to the anechoic lesion?
Diagnostic Considerations
As stated before, there are possibly two findings in this case that may not be related to each other: echogenic fetal kidneys and a cystic lesion in the fetal thorax. Since the fetal heart and lungs appear to be grossly normal, the source of the cystic lesion in the fetal chest remains in question. Therefore, a diaphragmatic hernia or even bronchogenic cysts should be considered.
A diaphragmatic hernia usually produces significant midline shift and also generally is located to the left side or, rarely, to the right of the mediastinum. Since this lesion is located in the middle, could it stem from bronchogenic cysts?
As previously noted, the fetal lungs appear to be grossly normal. Besides, bronchogenic cysts would be located either to the left or the right of the mediastinum and may be limited to the upper thorax. In this case, the cystic lesion is in the lower thorax. So, what can produce a midline cystic lesion in the lower thorax without producing significant shift of the fetal heart?
In these images, the fetal stomach is not fully visible in the fetal abdomen. This indicates a fetal hiatal hernia, which could explain all of the previously mentioned findings, which include:
⪠A small, anechoic lesion in the lower fetal chest.
⪠No significant midline shift or displacement of the heart to either side.
⪠A fetal stomach not well visualized within the confines of the abdominal cavity.
⪠Echogenic fetal kidneys.
The focus of these findings centers entirely around the location of the fetal stomach. The only possible condition that can cause a displacement of the stomach upwards into the fetal chest and along the midline would be a fetal hiatal hernia. This is a rare occurrence, as most hernias occur because of a large diaphragmatic defect on either the left or the right side.
Final Diagnosis
Fetal hiatal hernia with echogenic fetal kidneys
The incidental finding of enlarged, echogenic fetal kidneys possibly represents polycystic kidney disease and appears to be unrelated to the fetal hiatal hernia.
Discussion
The esophageal hiatus is an opening in the diaphragm that allows entry of the esophagus into the abdominal cavity to join the stomach. When the esophageal hiatus becomes enlarged, a part of the stomach herniates upwards through the hiatus into the thoracic cavity, causing a hiatal hernia.
There are three types of hiatal hernias: sliding, paraesophageal, and mixed. The most common variety is the sliding hiatal hernia, which is characterized by all or part of the stomach and the gastroesophageal junction herniating upwards into the thoracic cavity. The images in this case show all the typical features of a sliding hiatal hernia. In a paraesophageal hiatal hernia, the gastroesophageal junction is located normally and a part of the stomach herniates alongside the lower esophagus through the hiatus. Mixed hiatal hernias have characteristics of both sliding and paraesophageal hernias.
Congenital hiatal hernias are extremely rare. The chief diagnostic features of a hiatal hernia include:
⪠A midline cystic lesion in the lower thoracic cavity that is posterior to the heart and anterior to the fetal spine.
⪠Abnormally located stomach bubble, which connects with the cystic lesion in the thoracic cavity.
⪠A part or all of the fetal stomach may not be visualized in its normal location in the abdomen.
⪠Lack of significant midline shift or displacement of the fetal heart.
All of these features were present in this case and clearly differentiate the lesion visualized in the fetal thorax from a congenital diaphragmatic hernia.
Differential diagnoses: The main diagnoses of consideration for fetal hiatal hernia include congenital diaphragmatic hernia, congenital cystic adenomatoid malformation, bronchogenic cyst, and teratoma. In this case, the typical sonographic findings of fetal hiatal hernia help clearly differentiate this diagnosis from all other possible diagnoses.
References:
Yamamoto N, Hidaka N, Anami A, et al. Prenatal sonographic diagnosis of a hiatal hernia in a fetus with asplenia syndrome. J Ultrasound Med. 2007;26:1257-1261.
Rumack CM, Wilson SR, Charboneau JW, Levine D, eds. Diagnostic Ultrasound. 4th ed. Philadelphia: Mosby; 2011.
Cusick W, Bork MD, Bourque MD, et al. Hernia, hiatal. Available at: http://sonoworld.com/fetus/page.aspx?id=242. Accessed February 27, 2014.
S1E4: Dr. Kristina Adams-Waldorf: Pandemics, pathogens and perseverance
July 16th 2020This episode of Pap Talk by Contemporary OB/GYN features an interview with Dr. Kristina Adams-Waldorf, Professor in the Department of Obstetrics and Gynecology and Adjunct Professor in Global Health at the University of Washington (UW) School of Medicine in Seattle.
Listen
Unveiling the complexities of preterm birth risk from nativity, ethnicity, and race
March 22nd 2024A recent study dissected the relationships between maternal nativity, ethnicity, and race in influencing preterm birth rates, shedding light on disparities and suggesting avenues for future research.
Read More
Study reveals link between opioid dosage and spontaneous preterm birth risk
February 21st 2024Recent research highlighted an association between the total dose of prescribed opioids during pregnancy and the heightened risk of spontaneous preterm birth, emphasizing the need for judicious opioid use in pain management for expectant mothers.
Read More
